Choriocarcinoma During Pregnancy | Symptoms, Causes, Treatment
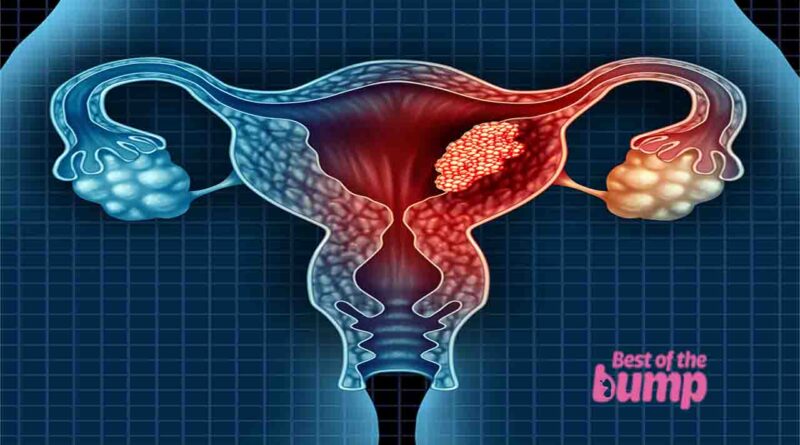
Choriocarcinoma is a rare and malignant tumor that originates from the tissue and cells that would typically develop into the placenta. It falls under the category of gestational trophoblastic diseases (GTD), which are a group of uncommon conditions characterized by the abnormal growth of cells in the uterus from the tissue formed after conception.
This particular type of GTD, choriocarcinoma, often arises following events such as a molar pregnancy, miscarriage, abortion, or ectopic pregnancy, where remnants of placental tissue persist and continue to grow despite the absence of a developing fetus. It can also occur after full-term delivery, although such instances are extremely rare, with choriocarcinoma happening in only 1 out of every 40,000 pregnancies. Given its infrequency, choriocarcinoma is considered a highly uncommon but serious medical condition that requires prompt attention and intervention.
What is choriocarcinoma?
Gestational choriocarcinoma is a rare type of tumor primarily affecting pregnant women, and it falls under the category of gestational trophoblastic disease (GTD). Unlike some other forms of GTD, a choriocarcinoma is malignant.
This cancer typically originates in the uterus but can have the potential to spread to other parts of the body. Due to its aggressive nature, early detection and prompt medical intervention are crucial for effective treatment and management. The unique association with pregnancy and its potential to metastasize set gestational choriocarcinoma apart as a distinct and specialized condition within the broader spectrum of gestational trophoblastic diseases.
What Causes It?
Choriocarcinoma develops when cells that would typically form the placenta during a normal pregnancy undergo a malignant transformation. The specific events that lead to the formation of choriocarcinoma are often associated with certain reproductive conditions, including:
- Miscarriage: Choriocarcinoma can occur after a miscarriage, which is the spontaneous loss of a pregnancy before the 20th week.
- Abortion: Both spontaneous (miscarriage) and induced (termination of pregnancy) abortions can be associated with the development of choriocarcinoma.
- Ectopic Pregnancy: Choriocarcinoma may arise after an ectopic pregnancy, where the fertilized egg implants outside the uterus, most commonly in the fallopian tube.
- Molar Pregnancy: A molar pregnancy occurs when an egg is fertilized, but the placenta develops into a mass of cysts instead of forming a fetus. Choriocarcinoma is particularly associated with molar pregnancies.
In these reproductive events, the placental tissue left behind can give rise to choriocarcinoma, where normal cells undergo abnormal and cancerous changes. The cancerous cells can then grow and potentially spread to other parts of the body. It’s important to note that choriocarcinoma is a rare condition, and not all pregnancies or reproductive events lead to its development. Early detection and appropriate medical intervention are crucial for effective treatment.
Who is most at risk for choriocarcinoma?
Certain factors can increase the risk of developing choriocarcinoma, and individuals with the following characteristics may be at a higher risk:
- Age: Women over the age of 40 have an increased risk of choriocarcinoma.
- Previous Molar Pregnancy: Individuals who have experienced a molar pregnancy, where fluid-filled sacs or tumors develop inside the uterus instead of a normal placenta during pregnancy, are at an elevated risk.
- Abortion: Women who have had an abortion may have an increased risk.
- History of Miscarriage: Individuals with a history of miscarriage may be at a higher risk.
- Ectopic Pregnancy: Those who have had an ectopic pregnancy, where a fertilized egg implants outside the uterus (commonly in the fallopian tube), are at an increased risk.
- Family History: Individuals with a family history of choriocarcinoma may be more susceptible.
- Ethnicity: The risk is higher in women of Asian or Native American descent.
It’s essential for individuals with concerns or those who fall into these risk categories to discuss their health history with their OB/GYN. Regular check-ups and open communication with healthcare professionals can help in monitoring and addressing potential risks promptly. Early detection and intervention are crucial for effective management and treatment of choriocarcinoma.
What are some symptoms of choriocarcinoma?
It’s crucial to be vigilant for signs of choriocarcinoma, especially if you’ve had a molar pregnancy, miscarriage, abortion, or ectopic pregnancy. Here are some symptoms to be aware of:
-
Continued Vaginal Bleeding
- Persistent vaginal bleeding after a molar pregnancy, miscarriage, abortion, or ectopic pregnancy. This bleeding may include blood clots or a watery brown discharge.
-
Abnormal Tissue Discharge
- Unusual tissue discharge may be a sign of choriocarcinoma.
-
Pelvic Pain or Discomfort
- Experience pelvic pain or discomfort, which could be indicative of underlying issues.
-
hCG Levels
- Elevated hCG (human chorionic gonadotropin) levels do not return to normal after the conclusion of a pregnancy.
If you have a history of ectopic pregnancy, miscarriage, abortion, or molar pregnancy, it is essential to attend regular follow-up visits with your healthcare practitioner. These visits are crucial for monitoring your health and ensuring proper healing.
If you notice any of the symptoms mentioned above within a year of the end of your pregnancy, it is important to discuss your concerns with your doctor promptly. Seeking medical attention early is vital for the timely diagnosis and management of choriocarcinoma. Regular communication with your healthcare provider is key to maintaining your overall health and well-being.
How Is It Diagnosed?
The diagnosis of choriocarcinoma typically involves a combination of clinical examinations and various tests to assess the presence of abnormal tissues and potential spread. The diagnostic process may include:
-
Pelvic Exam
- A pelvic exam is conducted to physically examine the pelvic area, feeling for any lumps or unusual changes that might indicate the presence of choriocarcinoma.
-
hCG Levels Test
- Measurement of levels of human chorionic gonadotropin (hCG) hormone through blood tests. Elevated levels of hCG may suggest the presence of a gestational trophoblastic disease (GTD), including choriocarcinoma.
-
Blood and Urine Tests
- Additional blood and urine tests may be performed to assess various markers and indicators related to the health of the reproductive system.
-
Physical Exam for Spread
- Examination to determine if the cancer has spread to other parts of the body. This may involve assessing nearby organs and tissues for signs of metastasis.
-
Imaging Tests
- Imaging tests such as CT (computed tomography), MRI (magnetic resonance imaging), ultrasound, or X-ray may be employed to visualize the uterus, surrounding structures, and potential metastasis. These tests help in determining the extent and location of the cancer.
The combination of these diagnostic methods allows healthcare professionals to gather comprehensive information about the presence, nature, and stage of choriocarcinoma. It’s important to note that an accurate diagnosis is crucial for planning an appropriate and effective treatment strategy. Once diagnosed, further tests may be conducted to determine the extent of the disease and guide treatment decisions.
What Is the Treatment?
After diagnosing choriocarcinoma, the next step is to determine the stage of the cancer. Staging involves assessing factors such as the size of the tumor, its extent of spread, and other characteristics. The staging helps in categorizing the cancer and guiding the appropriate treatment approach. Here are some key points about the treatment of choriocarcinoma based on its stage:
-
Low-Risk Choriocarcinoma
- If the tumor is classified as low-risk (small and localized without significant spread), chemotherapy is typically the primary treatment. Chemotherapy will be administered until there are no signs of cancer in the body, based on monitoring hCG levels.
-
High-Risk Choriocarcinoma
- In cases of high-risk choriocarcinoma, where the tumor is larger or has spread more extensively, the treatment approach may involve a combination of surgery, chemotherapy, and, in some cases, radiation therapy.
-
Treatment for Metastasis
- If the disease has spread to certain organs, such as the liver or the brain, additional considerations may be necessary. Treatment plans will be tailored to address the specific characteristics of each case.
-
Positive Prognosis
- The prognosis for choriocarcinoma is generally positive, especially when the cancer is detected early and appropriate treatment is initiated. Cure rates are high with prompt and effective management.
-
Individualized Treatment Plans
- Each case of choriocarcinoma is unique, and treatment plans are individualized based on the specific characteristics and staging of the cancer. The healthcare team, including oncologists and surgeons, will work with the patient to determine the most suitable and effective treatment strategy.
It’s crucial for individuals diagnosed with choriocarcinoma to work closely with their healthcare team, discuss treatment options, and receive ongoing monitoring and care. Regular follow-ups and communication with healthcare professionals are essential for tracking progress and ensuring the best possible outcome.
What can you do for your health if you have choriocarcinoma?
Joining a cancer support group, either online or in-person, can be a valuable source of information, comfort, and camaraderie for individuals diagnosed with choriocarcinoma. Here are some additional suggestions for coping and maintaining well-being during this challenging time:
-
Support Groups
- Consider participating in cancer support groups where you can connect with others facing similar experiences. Whether attending meetings in person or joining online forums, these groups provide a platform to share information, emotions, and support.
-
Self-Care
- Focus on taking care of yourself, both physically and emotionally. Prioritize self-care activities that bring comfort and relaxation.
-
Reach Out to Friends and Family
- Lean on your supportive network of friends and family. Sharing your journey with loved ones can provide emotional support and create a sense of community.
-
Healthy Lifestyle
- Follow a healthy diet and exercise routine, with guidance from your healthcare team. Research suggests that maintaining a balanced lifestyle, including regular exercise, stress relief practices like yoga and meditation, and a diet rich in whole grains, leafy green vegetables, legumes, and fruits, can positively impact health.
-
Coping with Rare Cancer
- Acknowledge the rarity of choriocarcinoma, but also take comfort in its high treatability and curability. Trust in your healthcare team, follow their guidance and maintain optimism about the positive outcomes achievable through treatment.
-
Focus on Recovery
- While facing challenges, maintain hope and focus on the prospect of recovery. Chances are good that with the support of your healthcare team and a strong support system, you will emerge from this experience healthy and cancer-free.
Remember that every individual’s journey is unique, and finding the right balance of emotional and practical support is essential. Engaging with healthcare professionals, participating in support groups, and maintaining a positive outlook can contribute to your overall well-being during the treatment and recovery process.
References
- National Institutes of Health, National Library of Medicine, Medline Plus, Choriocarcinoma Opens a new window, April 2022. | Show in the article
- National Institutes of Health, National Cancer Institute, Gestational Trophoblastic Disease Treatment Opens a new window, February 2022. | Show in the article
- What to Expect When You’re Expecting, 5th edition, Heidi Murkoff.
- Mayo Clinic, Dietary Fiber: Essential for a Healthy Diet Opens a new window, November 2022.
- National Institutes of Health, National Library of Medicine, Gestational Trophoblastic Disease, April 2022.