Cord Prolapse During Pregnancy
Cord prolapse stands out as a rare but significant risk associated with such situations, necessitating immediate medical attention to minimize the potential for severe complications.
Although the popular notion might associate the onset of labor with the dramatic event of the water breaking, the likelihood of experiencing premature rupture of the membranes—where the water breaks before contractions or active labor—is relatively low. In the event that this does occur, it is crucial to diligently follow the guidance provided by your healthcare provider.
What is cord prolapse?
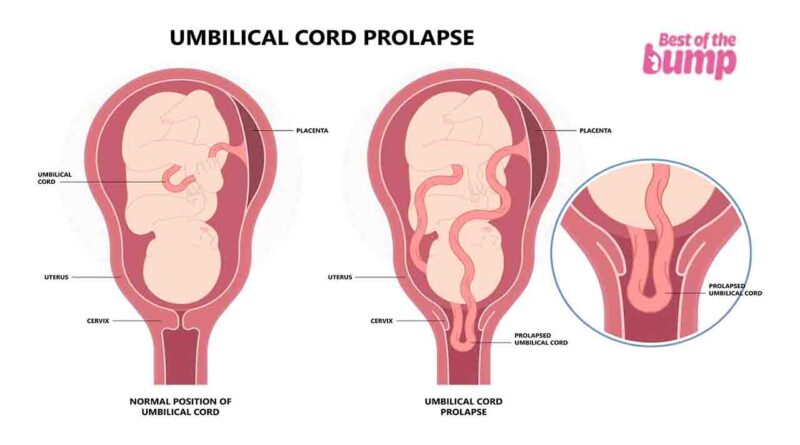
Cord prolapse occurs when the umbilical cord of an unborn baby slips through the cervix and into the vagina after the mother’s water breaks but before the baby descends into the birth canal.
During the delivery process, the prolapsed cord may become compressed by the baby’s body, potentially compromising the crucial oxygen supply from the placenta to the baby.
In the uncommon event of cord prolapse, prompt medical intervention is imperative. Delays in treatment increase the risk of complications, including placental abruption, excessive bleeding, fetal injuries, and the tragic outcome of stillbirth.
What causes cord prolapse?
Premature rupture of the membranes is a frequent precursor to cord prolapse, occurring when a mother’s water breaks before the onset of labor, and before her baby’s head has engaged or settled into the birth canal.
In some cases, medical interventions during labor can dislodge the baby’s head (or the part of the body facing downward), allowing the cord to slip past. Obstetric procedures contribute to around 50 percent of cord prolapse cases.
Who is most at risk for cord prolapse?
Various factors can contribute to the occurrence of cord prolapse during pregnancy and labor. These include your baby’s position, whether it’s breech, transverse, oblique, or an unstable lie, or if the head is unengaged in the pelvis. Other risk factors encompass preterm labor, low birth weight, carrying twins or multiples, having previous children, a low-lying placenta, atypical placental cord insertions, uterine malformations like fibroids, polyhydramnios (excessive amniotic fluid), a long umbilical cord, and prolonged labor.
Furthermore, obstetric interventions play a role in cord prolapse, particularly those associated with:
- Induction of labor, such as cervical ripening with a balloon catheter or artificial rupture of membranes.
- Use of forceps or a vacuum during delivery.
Understanding these risk factors and potential interventions is crucial for healthcare providers to effectively manage and minimize the risk of cord prolapse during pregnancy and childbirth.
How common is cord prolapse in labor?
Cord prolapse is a relatively uncommon occurrence, happening in approximately one out of every 300 births.
What are the symptoms of cord prolapse?
The primary symptom of cord prolapse is the sensation or visual identification of the prolapsed cord in the vagina or at the vaginal opening following the rupture of your amniotic sac. If you suspect cord prolapse, it is crucial to seek immediate medical attention by heading to the hospital or calling the Emergency Number. A healthcare provider will conduct a pelvic exam to confirm the presence of cord prolapse.
In a hospital setting, a doctor may raise suspicion of prolapse if your water has broken, and fetal monitoring indicates a decrease in your baby’s heart rate to less than 120 beats per minute. Timely recognition and intervention are essential in managing cord prolapse to minimize potential risks and complications.
How is cord prolapse treated?
If you suspect your baby’s umbilical cord is prolapsed and you are not already at the maternity ward, it is crucial to call the Emergency Number immediately or proceed to the hospital without delay. While waiting for medical assistance, assume a hands-and-knee position with your pelvis elevated and head down to alleviate pressure on the cord. During the car ride to the hospital, lying down with your hips elevated is recommended.
If you are already in the hospital when a cord prolapse occurs, your healthcare practitioner may instruct you to change positions to facilitate disengagement of your baby’s head and alleviate pressure on the umbilical cord.
Regardless of the situation, a swift delivery is imperative, often necessitating an immediate Cesarean section. Rapid delivery is typically the most effective measure to prevent potential complications associated with cord prolapse, including those arising from a lack of oxygen to the baby.
Is there anything you can do to prevent cord prolapse?
Indeed, the occurrence of cord prolapse is challenging to predict in advance. Despite identifiable risk factors, it’s important to recognize that cord prolapse can occur even in individuals with low-risk pregnancies delivering at term.
In cases where there are complications that heighten the risk of cord prolapse, healthcare providers may opt for a proactive approach by scheduling a Cesarean section. This strategy aims to minimize the likelihood of cord prolapse and its associated complications, providing a safer delivery environment for both the mother and the baby.
References
- National Institutes of Health, National Library of Medicine, Maternal Risk Factors and Outcomes of Umbilical Cord Prolapse: A Population-Based Study, January 2016.
- Cleveland Clinic, Umbilical Cord Prolapse Opens a new window, September 2020. | Show in the article
- March of Dimes, Umbilical Cord Conditions Opens a new window, June 2016. | Show in the article
- What to Expect When You’re Expecting, 5th edition, Heidi Murkoff.
- WhatToExpect.com, Polyhydramnios (Hydramnios) During Pregnancy, December 2020.
See this also –
- Chorioamnionitis During Pregnancy | Intrauterine infection
- Fifth Disease During Pregnancy
- Gestational Diabetes and Pregnancy
- Breech Position | What It Means if Your Baby Is Breech
- Choriocarcinoma During Pregnancy | Symptoms, Causes, Treatment
- Cord Knots During Pregnancy