Deep Vein Thrombosis (DVT) During Pregnancy and Postpartum
You might be familiar with certain pregnancy complications such as gestational diabetes and preeclampsia. However, there’s another relatively prevalent complication that warrants attention due to its potential for serious consequences: blood clots.
Deep vein thrombosis (DVT) is a form of a blood clot that occurs more frequently in pregnant women and can escalate to a more severe condition known as pulmonary embolism (PE). The good news is that both DVT and PE are manageable and even preventable, especially among women identified as being at higher risk. It’s essential to note that many mothers with blood clotting conditions still go on to have perfectly healthy pregnancies and deliveries.
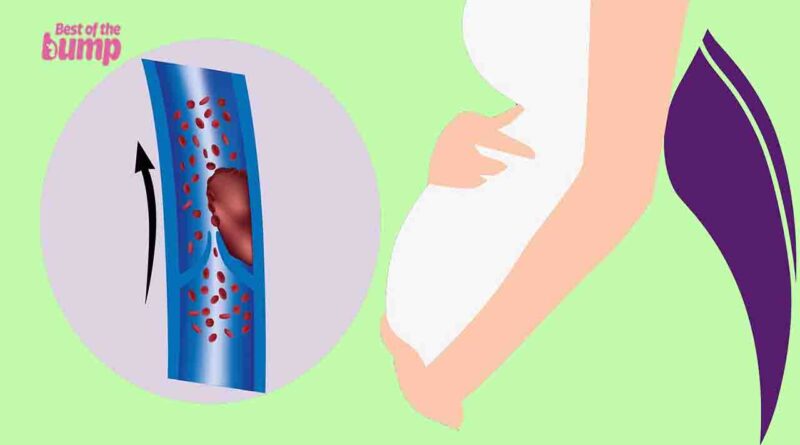
What is deep vein thrombosis (DVT)?
Deep vein thrombosis (DVT) is the formation of a blood clot in a deep vein. In the context of pregnancy, approximately 90 percent of DVT incidents manifest in the left leg. Swift intervention is crucial as it can prevent a clot from dislodging and journeying through the circulatory system to the lungs, a condition known as pulmonary embolism (PE), which poses a potential threat to life. Early detection and treatment are paramount in mitigating the risks associated with DVT during pregnancy.
How common is deep vein thrombosis (DVT)?
Venous thromboembolism (VTE), encompassing both deep vein thrombosis and pulmonary embolism, affects approximately two in every 1,000 pregnancies.
Despite being considered a relatively uncommon complication, VTE occurs about four to five times more frequently in pregnant women compared to other women of the same age. The risk further increases to 20 times more during the six weeks following childbirth. It’s noteworthy that, typically, by eight weeks postpartum, the risk of VTE should revert to normal levels. Understanding and monitoring these risks is crucial for the well-being of both expectant and postpartum women.
What are the signs of deep vein thrombosis (DVT) during pregnancy and postpartum?
The primary symptoms of deep vein thrombosis (DVT) during pregnancy and the postpartum period typically manifest in a single leg and include:
- A sensation of heaviness or pain in the leg: Often described as akin to a persistent, intense muscle strain.
- Tenderness, warmth, and/or redness in the calf or thigh: Observable signs of inflammation in the affected area.
- Slight to severe swelling: Swelling may be evident, varying in intensity.
If the blood clot progresses to the lungs, resulting in pulmonary embolism (PE), additional symptoms may arise:
- Chest pain exacerbated by deep breaths or coughing: Pain in the chest that intensifies with specific respiratory actions.
- Unexplained shortness of breath: Difficulty breathing that is not readily attributable to other factors.
- Coughing up blood: Hemoptysis, the act of coughing up blood.
- Rapid or irregular heartbeat: An abnormal or accelerated heart rate, potentially indicative of a serious condition.
Recognizing and promptly addressing these symptoms is crucial for the early detection and management of deep vein thrombosis during pregnancy and the postpartum period.
Why is deep vein thrombosis (DVT) more common in pregnancy and postpartum?
Deep vein thrombosis (DVT) may be more prevalent during pregnancy due to nature’s adaptive mechanism to limit bleeding during childbirth, leading to an increase in the blood’s clotting ability, sometimes to an excessive extent.
During pregnancy, there is a natural elevation in the levels of blood-clotting proteins, coupled with a decrease in anti-clotting protein levels. This shift in the clotting balance can contribute to the occurrence of DVT. Additionally, factors such as an enlarged uterus can amplify pressure on the veins responsible for returning blood from the lower body to the heart. Bed rest or limited movement during pregnancy can further contribute to the risk of developing DVT.
Understanding these factors is crucial in recognizing the potential risk of DVT during pregnancy and underscores the importance of appropriate medical monitoring and preventive measures.
Who is most at risk for deep vein thrombosis (DVT)?
The risk of deep vein thrombosis (DVT) is higher if you:
- Have a Family or Personal History of VTE (Venous Thromboembolism): A history of blood clotting issues in your family or a personal history of VTE increases the risk.
- Have Thrombophilia: Thrombophilia, an inherited blood clotting disorder, can elevate the risk of DVT.
- Are Overweight or Obese: Excess weight is associated with an increased risk of DVT.
- Smoke: Smoking is a risk factor for DVT as it affects blood circulation and clotting.
- Are on Strict Bed Rest: Prolonged bed rest or immobility increases the likelihood of blood clot formation.
- Have Preeclampsia: Preeclampsia during pregnancy is associated with an elevated risk of DVT.
- Have Certain Chronic Illnesses: Conditions such as hypertension, diabetes, inflammatory bowel disease, or other vascular diseases can contribute to the risk of DVT.
- Delivered by Cesarean Section: The surgical procedure of cesarean section increases the risk of DVT compared to vaginal delivery.
- Experience Postpartum Hemorrhage or Need a Blood Transfusion: Complications such as postpartum hemorrhage or the need for a blood transfusion can increase the risk of DVT.
Awareness of these risk factors is crucial during pregnancy and postpartum, and individuals with these risk factors may need closer monitoring and preventive measures to mitigate the risk of DVT. Consultation with healthcare professionals is essential for personalized guidance and risk assessment.
Can you prevent deep vein thrombosis (DVT)?
It’s important to inform your doctor if you have a clotting disorder or a family history of blood clots. Being aware of the signs of a blood clot is crucial, as early treatment can mitigate the risks of complications such as pulmonary embolism (PE).
To help prevent clots and deep vein thrombosis (DVT) during pregnancy, consider the following measures to promote healthy blood flow:
- Engage in Pregnancy-Safe Exercise: With approval from your healthcare provider, incorporate safe and suitable exercises into your routine to enhance blood circulation.
- Avoid Prolonged Sitting: If sitting for an extended period, such as during a flight, take breaks to walk and stretch every two to three hours.
- Leg Movements While Sitting: Keep blood flowing by regularly moving your legs while sitting—raise and lower your heels and toes.
- Take Precautions During Travel: Stay hydrated, take regular breaks to walk or stretch your legs, especially during travel.
- Consider Support Hose: If you are at a high risk, your doctor may suggest wearing support hose, although their effectiveness in preventing blood clots is not conclusively proven.
- Follow Medical Recommendations: If at a high risk, your healthcare provider might recommend a preventive dose of the blood thinner heparin (or low molecular weight heparin). This may be prescribed for the entire pregnancy or for several weeks after childbirth. Both types of medication are safe during pregnancy as they do not cross the placenta.
Adhering to these preventive measures and staying vigilant for potential symptoms can contribute to a healthier pregnancy and reduce the risks associated with blood clots and DVT. Always consult with your healthcare provider for personalized advice based on your individual circumstances.
Does DVT during pregnancy have any effects on your baby?
Deep vein thrombosis (DVT) is a type of venous thromboembolism (VTE), a term encompassing blood clots in any vein. VTE has been associated with preeclampsia, a condition that, while many individuals with it experience healthy pregnancies and deliver thriving babies, can lead to complications if left untreated.
Approximately 15 to 20 percent of DVT cases are linked to antiphospholipid syndrome (APS), an autoimmune disorder that heightens the risk of blood clot formation. APS is considered a form of thrombophilia, indicating a tendency to develop blood clots. This syndrome has connections to an increased risk of recurrent miscarriage, blood clots in the placenta, placental insufficiency (reduced efficiency in delivering food and oxygen to the baby), intrauterine growth restriction (IUGR), and potential heart attack and stroke in the mother.
If you have a history of blood clots or recurrent miscarriages, it’s crucial to inform your doctor. They may recommend blood tests to assess for antiphospholipid syndrome and take appropriate measures to monitor and manage the associated risks during pregnancy. Regular communication with your healthcare provider is vital for a comprehensive understanding of your individual risk factors and appropriate medical guidance.
When to see your doctor
If you or a close family member, such as a parent or sibling, has a history of deep vein thrombosis (DVT), it’s important to inform your healthcare provider. Your doctor may conduct a blood test to check for thrombophilia, a condition that increases the risk of blood clots. If thrombophilia is detected, your doctor may consider initiating blood thinners as a precautionary measure.
Should you observe any symptoms associated with DVT, especially during pregnancy or within the initial eight weeks after childbirth, it’s crucial to contact your practitioner promptly. Your doctor may conduct diagnostic tests, including blood tests, ultrasound, or other imaging tests, to confirm the presence of DVT or pulmonary embolism (PE).
If a blood clot is identified, your practitioner is likely to prescribe the blood-thinning medication heparin to reduce the blood’s clotting ability and prevent further clot formation. Special arrangements may be made as you approach labor to avoid excessive bleeding during childbirth while on heparin. Throughout the process, your doctor will closely monitor your blood clotting ability to ensure optimal management and a safe pregnancy. Regular communication with your healthcare provider is essential for effective monitoring and timely intervention.
References
- American College of Rheumatology, Antiphospholipid Syndrome Opens a new window, March 2019.
- American Family Physician, Venous Thromboembolism During Pregnancy Opens a new window, June 2008.
- What to Expect When You’re Expecting, 5th edition, Heidi Murkoff.
- WhatToExpect.com, 13 Benefits of Exercise During Pregnancy, October 2018.
- American College of Obstetricians and Gynecologists, Preventing Deep Vein Thrombosis, Opens a new windowMarch 2020.
- Centers for Disease Control and Prevention, Venous Thromboembolism (Blood Clots) and Pregnancy Opens a new window, August 2020.
- Mayo Clinic, Deep Vein Thrombosis (DVT) Opens a new window, July 2018.
- National Institutes of Health, National Library of Medicine, Antiphospholipid Syndrome Opens a new window, August 2020.
- Obstetrics and Gynecology, ACOG Practice Bulletin No. 196: Thromboembolism in Pregnancy Opens a new window, July 2018.