Cytomegalovirus (CMV) During Pregnancy
Cytomegalovirus (CMV) is a highly prevalent viral infection, with research indicating that nearly one in three children in the United States contracts the virus by the age of 5. This suggests that there’s a high likelihood of having been infected in the past without exhibiting noticeable symptoms, and the potential impact on pregnancy is generally considered low.
Due to the uncertain risk of CMV affecting a baby during pregnancy, routine testing is not commonly conducted by doctors. Nevertheless, it’s crucial to inform your healthcare provider if you suspect a CMV infection during pregnancy, particularly if you have frequent interactions with young children. Although rare, CMV can lead to serious complications for newborns after birth.
What is Cytomegalovirus (CMV)?
CMV, short for cytomegalovirus, is a common and persistent virus. According to the Centers for Disease Control and Prevention (CDC), one in three children contracts CMV by the age of 5, and over half of adults have the virus by age 40.
Once you acquire Cytomegalovirus (CMV), it stays with you for life, often lying dormant in your body after the initial infection. Detecting CMV can be challenging because it frequently operates without causing noticeable symptoms. Many infected individuals are unaware of their CMV status.
Cytomegalovirus (CMV) infections can be categorized into three types:
- Acute CMV: Some individuals experience flu-like symptoms such as fever, fatigue, and aches.
- CMV in Immunocompromised Individuals: Those with weakened immune systems may develop severe CMV-related diseases affecting areas like the eye, brain, and digestive tract.
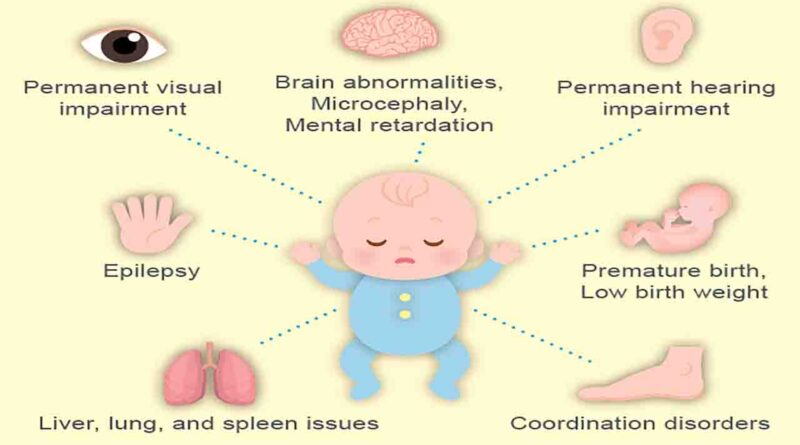
- Congenital CMV: Babies can contract CMV in the womb, potentially leading to significant health or developmental issues. Around one in five babies born with congenital CMV may face long-term health problems.
The risk of CMV during pregnancy, particularly congenital CMV, is a significant concern. It can pose potential threats to the developing baby, with about one in five babies born with congenital CMV experiencing lasting health challenges. Understanding these risks is crucial for expectant mothers to ensure proper monitoring and intervention if needed.
Why is CMV a risk during pregnancy?
It’s important to note that CMV is highly prevalent, with the CDC estimating that nearly half of pregnant individuals have encountered CMV before their first pregnancy. About 1 to 4 percent of others may acquire the infection at some point during pregnancy.
If you have CMV, there’s a risk of transmitting the virus to your baby, as the virus present in your blood can reach the developing baby through the placenta. The likelihood of transmission is higher if you contract the virus during pregnancy, but it can still occur if you had CMV before becoming pregnant, although less commonly.
The significance of CMV as a risk during pregnancy lies in the potential for serious complications when the virus is passed to the developing baby, with severe cases even leading to pregnancy loss.
When a baby is born with CMV, it is termed congenital CMV, indicating a condition present from birth. The CDC estimates that 1 in 200 babies is born with congenital CMV. These infants may experience various short- and long-term health complications, including low birth weight, skin rash, jaundice, enlarged liver or spleen, microcephaly (smaller-than-average head size), seizures, hearing loss, vision loss, intellectual disabilities, and developmental delays. Understanding and addressing the risks associated with CMV during pregnancy is crucial for safeguarding maternal and infant health.
What are the symptoms of CMV?
A majority of individuals infected with CMV do not exhibit any symptoms, a condition referred to as being asymptomatic. Consequently, most pregnant individuals with CMV may remain unaware of their infection.
In some cases, individuals who contract CMV during pregnancy might experience symptoms indicative of an acute infection. These symptoms can include:
- Fever, with or without chills
- Fatigue
- Body aches and pains
- Headache
- Swollen lymph nodes
The challenge lies in the nonspecific nature of these symptoms, making it easy to mistake them for other types of infections such as the flu or infectious mononucleosis. As a result, the absence of overt symptoms can contribute to a lack of awareness regarding CMV infection, particularly during pregnancy.
What causes CMV?
CMV belongs to the herpesvirus family and is specifically known as human herpesvirus-5 (HHV-5).
While the terms “herpesvirus” often bring to mind herpes simplex viruses 1 and 2, responsible for oral and genital herpes, the herpesvirus family encompasses a diverse range of viruses. Alongside CMV and herpes simplex viruses, this family includes several other viruses associated with well-known health conditions, such as:
- Varicella-zoster virus, responsible for chickenpox and shingles
- Epstein-Barr virus, which causes infectious mononucleosis
- Kaposi’s sarcoma-associated herpesvirus (KSHV), is linked to the development of Kaposi’s sarcoma, a form of cancer.
Understanding the diversity within the herpesvirus family is crucial in recognizing the various health conditions caused by these viruses.
How do you get CMV?
CMV spreads through direct contact with body fluids containing the virus, including:
- Blood
- Urine
- Semen
- Vaginal fluids
- Saliva
- Tears
- Breast milk
Transmission can occur if you come into direct contact with any of the aforementioned body fluids and then touch your nose, mouth, or eyes. Additionally, CMV can be transmitted from person to person through various means such as:
- Pregnancy and labor
- Nursing
- Kissing
- Handling dirty diapers
- Sexual contact
- Sharing personal items like toothbrushes, eating utensils, or cups
- Receiving a blood transfusion, organ transplant, or bone marrow transplant from an individual with CMV
Being aware of these modes of transmission is essential for taking preventive measures and minimizing the risk of CMV infection.
How is CMV diagnosed?
Laboratory tests can determine the presence of CMV in your system, often by checking for CMV antibodies in your blood. Despite the availability of these tests, it’s uncommon for doctors to conduct CMV testing during pregnancy. This might seem counterintuitive, but several reasons contribute to this approach:
- Limited Predictive Capability: A positive result indicates the presence of CMV but cannot predict whether the virus will be transmitted to your baby or if they will experience long-term health issues.
- Interpretation Challenges: Test results can sometimes be challenging to interpret, making it difficult to determine if the CMV infection occurred recently or not.
- Effectiveness of Medications: Although medications exist for treating CMV in adults or children, there’s insufficient evidence to demonstrate their efficacy in preventing transmission to a developing baby.
While routine Cytomegalovirus (CMV) testing is not standard, there are situations where your doctor may recommend it. This includes instances where you believe you’ve been exposed to CMV or if your doctor suspects an acute CMV infection.
If testing is recommended and you test positive for Cytomegalovirus (CMV), additional assessments may follow. Your doctor might suggest testing the developing baby for the virus through procedures like amniocentesis, involving the collection and analysis of amniotic fluid. Additionally, an ultrasound may be conducted to identify potential signs of congenital CMV. These measures are taken to assess and manage potential risks associated with CMV infection during pregnancy.
What is the treatment for Cytomegalovirus (CMV)?
Cytomegalovirus (CMV), like all herpesviruses, lacks a cure, and once contracted, it persists for life.
As of now, there is no approved treatment specifically for CMV during pregnancy. Although antiviral medications may help manage the infection, they do not always guarantee the prevention of virus transmission to the developing baby.
Ongoing research is exploring the safety and effectiveness of various antiviral medications in preventing Cytomegalovirus (CMV) transmission during pregnancy. Encouragingly, some results, such as those from a small 2020 clinical trial, suggest that the antiviral medication valaciclovir (Valtrex) may be both safe and effective.
In cases where babies are born displaying signs of congenitalCytomegalovirus (CMV), antiviral medications are administered. This treatment aims to reduce the risk of long-term health complications in affected infants. While a definitive cure remains elusive, advancements in research offer potential avenues for managing and mitigating the impact of CMV infection, particularly in newborns.
What are the risk factors for Cytomegalovirus (CMV)?
Many people get CMV when they’re still young. That’s why CMV is often found at high levels in the saliva and urine of babies and young children.
Direct contact with these fluids can increase your risk of getting Cytomegalovirus (CMV). Generally speaking, individuals who live or work with young children are at a higher risk of contracting CMV in this way.
With this knowledge in hand, you can take steps to avoid Cytomegalovirus (CMV) while you’re pregnant by doing the following:
- thoroughly washing your hands with soap and water after:
- changing a child’s diaper
- feeding a child
- wiping a child’s eyes or nose
- picking up a child’s toys
- not sharing food, cups, or eating utensils with babies and young children
- avoiding contact with saliva and tears when kissing children, trying to kiss them on the head or cheek instead
Additionally, since CMV can also be spread through sex, consider using a condom or other barrier method during sex if you know that your partner has CMV.
What’s the outlook for people with CMV?
The likelihood of transmitting Cytomegalovirus (CMV) to your child is higher if you contract the virus during pregnancy, with the risk escalating to 40 to 70 percent by the third trimester.
The timing of Cytomegalovirus (CMV) contraction is a critical factor in the potential outcomes. Contracting the virus early in pregnancy, typically before 20 weeks, is associated with more severe effects.
Even individuals who acquired CMV before pregnancy can transmit the virus, but the risk of transmission is considerably lower approximately 3 percent.
For those who already have CMV, there are two situations during pregnancy where transmission is more likely:
- Reactivation: If the virus, typically in a dormant state, becomes active during pregnancy, viral particles can enter the bloodstream and reach the placenta.
- Reinfection: There is also a risk of reinfection if you contract a different strain of CMV from the one you already have.
It’s worth noting that not all babies born to mothers with CMV will face health concerns, as about 90 percent do not experience issues at birth. However, of those who do, 40 to 60 percent may develop long-term health complications.
Timely intervention with antiviral medications can contribute to improving outcomes for infants with congenital CMV, emphasizing the importance of early detection and treatment.
Frequently Asked Questions about Cytomegalovirus (CMV)
Cytomegalovirus (CMV)
What does Cytomegalovirus (CMV) do to the body?
CMV, like other herpesviruses, can enter a dormant state, periodically reactivating. During reactivation, viral particles may temporarily be present in blood and body fluids, potentially leading to transmission.
What are the long-term effects of Cytomegalovirus (CMV)?
In adults, CMV typically poses minimal risks unless they are immunocompromised or have specific medical conditions. However, babies born with congenital CMV can experience lasting effects, including hearing loss, vision loss, and intellectual disabilities. CMV is a primary cause of non-genetic hearing loss at birth.
Is CMV a sexually transmitted infection (STI)?
CMV can be considered an STD since it can be transmitted through sexual contact. However, it’s important to note that CMV can also spread through other means.
Is CMV related to COVID-19?
No, CMV and SARS-CoV-2, the virus causing COVID-19, are distinct viruses. CMV belongs to the herpesvirus family with DNA as its genetic material, while SARS-CoV-2 is a coronavirus with RNA as its genetic material. They differ in transmission methods and effects on the body.
The Takeaway
CMV is a common virus among adults, potentially causing serious complications during pregnancy, particularly congenital CMV. The highest risk of transmission occurs when individuals contract the virus for the first time during pregnancy. While most people aren’t routinely screened for CMV during pregnancy, those with concerns or symptoms should consult healthcare professionals for guidance on further steps and potential interventions. As of now, there are no approved treatments specifically designed to prevent CMV transmission during pregnancy.
References
- Centers for Disease Control and Prevention, About Cytomegalovirus: CMV Opens a new window, August 2020.
- Centers for Disease Control and Prevention, CMV Fact Sheet for Pregnant Women and Parents Opens a new window, September 2018.
- Centers for Disease Control and Prevention, Babies Born With Congenital Cytomegalovirus (CMV) Opens a new window, May 2022.
- Centers for Disease Control and Prevention, About Infectious Mononucleosis, September 2020.
- National Health Service, Cytomegalovirus (CMV), October 2020.